A Blood Glucose Meter is a Must in Your Diabetes Toolbox
Blood Glucose Meter is a Must in Your Diabetes Toolbox
If you are a person living with diabetes you are aware of the self-care required on a daily basis. It can be tiresome at times. Your daily routine should consist of monitoring your blood glucose levels. You may also be taking medications. You may also be planning your meals and activity. This all helps with the success of self-managing diabetes. Also, having a blood glucose meter is a must in your diabetes toolbox.
If you are only checking your blood glucose once a day and are taking oral medications, you might be okay using a regular blood glucose meter (BGM). You may consider using a continuous glucose monitor (CGM) if you are checking your levels multiple times throughout the day. You may also be using a continuous glucose monitor (CGM) if you are using daily injections of insulin or using an insulin pump.
Why You Always Need a Blood Glucose Meter (BGM)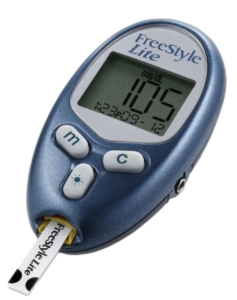
It’s important to note that a continuous glucose monitor (CGM) does not and should not replace a regular blood glucose meter (BGM). You should measure your blood sugar twice a day to make sure your continuous glucose monitor (CGM) is accurate, or during setup of your CGM. You should always have a blood glucose meter (BGM) and test strips on hand, it is critical to have handy for testing. Plan to always keep one in your travel bag. You never know when you may need it! For a person living with diabetes, having a blood glucose meter is a must in your diabetes toolbox.
You need to remember glucose usually moves into your blood vessels and capillaries first and then into your interstitial fluid. So, the sensor readings may lag behind the blood glucose readings to some extent. It’s like a roller coaster effect. The blood and sensor readings are expected to be different. A greater difference between blood and sensor readings will be seen when your glucose is changing quickly. This would happen after eating or after taking a bolus of insulin, or when you are ill or very stressed. During these times, when you need to know what your blood glucose levels are you must use your blood glucose meter (BGM). It is more accurate if you need to make a treatment decision.
Know the Differences
A CGM measures the amount of glucose in the fluid inside your body. Different devices collect this information with the use of small sensors placed on the body that contain a tiny canula inserted below the skin. It will attach at the back of your arm or on your abdomen. A transmitter on the sensor sends the information to a receiver device or your phone approximately every 5 minutes. The value of the CGM is that it gives you trends. You will see arrows alongside your reading. This lets you know where your glucoses heads. This insight will let you take the appropriate action to prevent episodes of hyper or hypoglycemia. This helps you to stay in your target range or time in range (TIR). Time in range is a fairly new measurement used with CGMs that track the percent of time your blood sugar is between the target range of 70 – 180mg/dL. According to the American Diabetes Association (ADA), most people with type 1 and type 2 diabetes should aim for a target TIR of at least 70% of readings or about 17 out of 24 hours per day.
A fingerstick glucose reading is a snapshot in time, whereas the CGM is a motion picture event. The CGM shows you the patterns and trends needed to identify what changes may be necessary in your diabetes management.
In summary, both tools are important to have in your toolbox since blood glucose levels can change based on the day you are having. Use your CGM to get the big picture but keep your BG meter ready for those unexpected situations that may arise like illness, or CGM malfunction. It’s always better to be prepared. This little device, the blood glucose meter is a must have in your diabetes toolbox.




